An operation to detach and re-join the ureter to the bladder. Also termed “ureteral reimplant”. This operation changes the way an abnormal ureter connects with the bladder.
What is Vesicoureteric Reflux & VUJ Obstruction Treatment Ureteric Reimplantation?
How does the urinary system work?
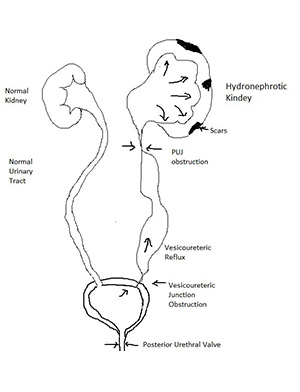
The urinary system consists of the kidneys, ureters, the bladder and urethra. The kidneys filter the blood to remove waste products and produce urine.
The urine flows from the kidneys down through the ureters to the bladder, where It’s stored until we go to the toilet. It passes through another tube called the urethra to the outside when urinating (peeing).
The ureter should run through the bladder wall at an angle, to form a tunnel. This tunnel is compressed when the bladder is full, preventing urine from washing back up to the kidney. If the ureter enters the bladder abnormally, there can be problems – usually because the tunnel is too short or too narrow.
What are the conditions that require surgery?
Tunnel too short = Vesicoureteric Reflux (VUR)
If the tunnel is too short, urine can wash back up to the kidney. This is not usually a problem, unless the child is also prone to recurrent urinary infections. In these cases, the kidneys can be affected by the infection being washed back up by the reflux. If the infections cannot be controlled, the reflux may need to be corrected by surgery.
Tunnel too narrow = Vesicoureteric Junction Obstruction (VUJO)
Some children have narrowing or blockage at the join between ureter and bladder. If surgical treatment is indicated, this is also often by way of a reimplantation operation.
What happens next?
The child is admitted on the day of surgery and the operation performed under general anaesthesia. The child should not eat or drink at least 6 hours before the surgery. If the child is breastfed, last feed should be given at least 4 hours before the surgery. If you do not follow this your operation can be delayed or cancelled.
A dose of antibiotics is given to reduce the chance of urinary tract infection.
What are the different modes of surgery?
The operation will be performed by robotic assisted keyhole surgery. This is the most advanced and would give results on par or better when compared to open surgeries. We would recommend your child to have a robot assisted surgery for best result. Other way will be to have an open surgery.
Please follow the link on Paediatric Robotic Surgery to know more.
For VUR repair, the tunnel is made longer and tighter to prevent backing up of urine. When performed by an experienced surgeon, it is 95% successful at correcting the reflux. There are other less invasive treatments, such as the injection of bulking agents (eg. Deflux) to narrow the tunnel. These are less successful overall than a reimplantation, particularly for severe cases. They do have a role in selected cases
For VUJ obstruction, new tunnels are made between the lining of the bladder and the bladder muscle, mimicking the normal state. The ureters are laid in these tunnels and secured to the bladder with dissolving stitches. When performed by an experienced surgeon, it is 98% successful at correcting the blockage. There are other, less invasive techniques that may be considered. Dilatation with a balloon device, after partial cutting of the inside of the narrowed tunnel is appropriate in selected cases. Your surgeon will be able to discuss the benefits of each technique with you in regards to your child.
To support the new join between ureter and bladder, and help it heal in the right position, a ‘stent’ is commonly left inside for a period of time. A stent is a fine plastic tube, which runs from a curl in the renal pelvis to a curl in the bladder. It acts like a straw (helps urine drain through the area of swelling) as well as a splint (to help the join heal in optimal position). This is a temporary device, removed 4-6 weeks after surgery. A catheter (tube) is often left in the bladder for 24 to 48 hours after surgery. This usually drains blood-stained urine. It would be removed before your child is ready to go home. Regular oral pain relief is given. Your child is discharged home once drinking and voiding. Bladder spasms are common for about 5 days after surgery. There are few medications that help, but reassurance and warm baths do.
Book your appointment online
Schedule your visit online without any hassle by filling the form. Simply put in your details and our representative will get back to you in 24 hours.
What are the complications?
As with any operation, bleeding and infection are the most frequent complications to occur. These are uncommon after reimplantation. Bleeding is the form of haematuria (blood in the urine) is expected for up to 2 weeks after the surgery. In the absence of blood clots, this is usually self-limiting and rarely represents significant blood loss. Infection in the urine or wound is possible. This may present with fever, dysuria (pain with voiding), frequency (needing to void often) or urgency. The wound may become red or swollen.
Complications Specific to Ureteric Reimplantation
The most likely complication (<5%) is the failure to fix the reflux. This would be looked for if child continued to have kidney infections following surgery.
If no stent is used, swelling at the site of the new join (anastomosis) may impede urine passage into the bladder after surgery, causing early blockage. A tube may need to be placed directly into the kidney (nephrostomy) until the swelling settles. This problem is usually prevented by use of internal stent. In the longer term, obstruction (blockage) due to scarring of the new tunnels is also possible. The chance of this is small (<1%) and is looked for with postoperative ultrasounds.
A urine leak from new joins is possible, but this is very uncommon. It would be suspected in a child with increasing pain, nausea, or fever. A drain may need to be placed till the leak heals on its own. If this doesn’t become alright, a repeat surgery to correct leak may be needed.
What happens next?
First follow-up event is removal of the internal stent(s). This will be arranged for 4-6 weeks after surgery. It will involve a day procedure where a cystoscopy (telescope) is performed to snare the stent(s) in the bladder and withdraw it. A brief general anaesthetic is given, but no further cuts or stitches are required. The next follow-up will be one month following stent removal, with another ultrasound performed a day or two prior to the clinic visit. Please ensure that you bring all new and old ultrasound pictures with you to clinic. Further follow-up will depend on this ultrasound and will be discussed at the clinic appointment.

